Special K: The Unexpected Antidepressant
Kaiya Bhatia
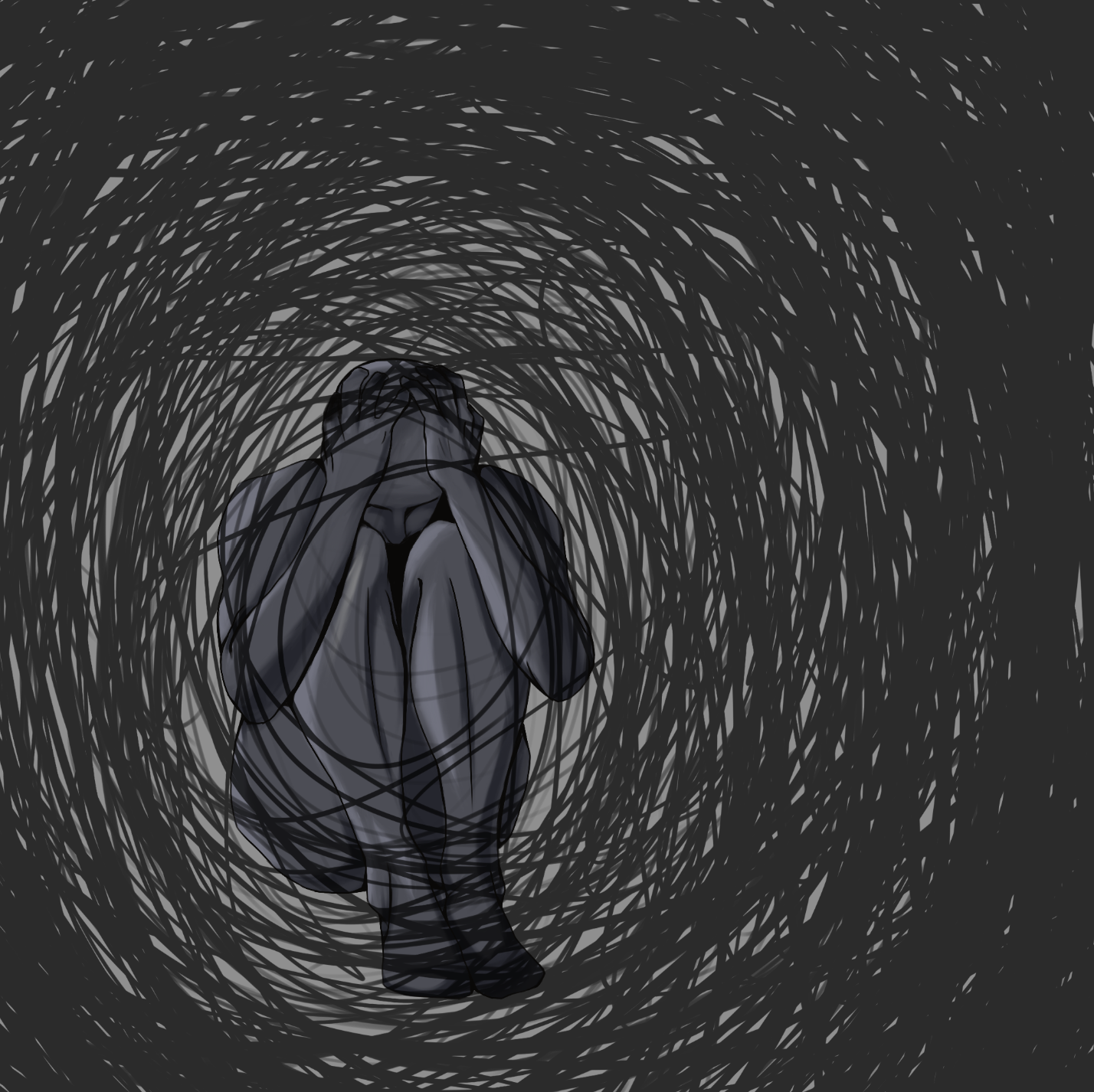
Illustrations by Ella Kolk
Did you know that Special K could be the key to effectively treating depression? No, we’re not talking about cereal, we’re talking about ketamine. Similar to other psychedelic drugs, like LSD and hallucinogenic mushrooms, high doses of ketamine can cause altered consciousness and changes in self-perception [1]. However, while you may think of ketamine as merely an illicit club drug or hallucinogen, it actually serves a variety of medical purposes. Ketamine was first introduced to the world of medicine as an anesthetic, preventing patients from processing sensory information [4]. More recently, however, ketamine has demonstrated great promise as a novel treatment for major depressive disorder (MDD) [2]. This common mental health condition causes patients to experience persistent feelings of sadness, often coupled with the loss of interest in daily activities; frustratingly, the treatments widely used for MDD have major drawbacks [2, 3]. Ketamine, however, offers a new way of addressing debilitating depressive symptoms, potentially without the concerns of safety and efficacy that are typical of traditional antidepressants.
You may be wondering how ketamine could travel from the floors of operating rooms and chic dance clubs to a psychiatric clinic near you. About 20 years ago, it was found that lower doses of ketamine could also be used to treat symptoms of MDD [5]. Drugs that activate the same brain receptors as ketamine have antidepressant effects, suggesting that ketamine does the same [6, 5]. Based on these findings, psychiatrists began to use ketamine as an emergency treatment for suicidal ideation due to its fast-acting properties and lack of harmful side effects characteristic of traditional depression treatments such as higher rates of suicidal ideation [7, 8]. Because of these properties, ketamine may potentially constitute our best treatment for MDD yet [2]. But what neural mechanisms underlie these crucial differences that cause ketamine to work better than traditional treatments for MDD? Let’s delve into the neuroscience behind the miraculous antidepressant qualities of “Special K.”
Putting the “Special” in Special K
The most common treatments for depression today are selective serotonin reuptake inhibitors (SSRIs), or drugs that increase the concentration of serotonin in the brain. Serotonin is a neurotransmitter, or chemical messenger, that helps regulate our mood by sending messages of satiation throughout the brain via neuronal, or brain cell, communication. In order for serotonin to work as a mood regulator, it is first released by one neuron into the small space that sits between the original neuron and another one nearby. This space is called the synapse. The nearby neuron then receives some of the serotonin, thereby getting the message of satisfaction. However, once the message is appropriately received, some serotonin remains in the synapse. To bring back this remaining serotonin so that it can be re-used for later signaling, the original neuron undergoes a process called “reuptake,” pulling the leftover serotonin back into the cell. This is where SSRIs come in: they block reuptake and prevent the disappearance of serotonin from the synapse. Think of SSRIs like a plug in a bathtub. When you plug a drain, all the water remains in the tub rather than disappearing down the pipes. Similarly, SSRIs “plug” the reuptake mechanism so that serotonin remains in the synapse rather than disappearing back into the cell. Ketamine treatment, however, combats depression differently.
Understanding the complex biochemistry of ketamine can seem a bit overwhelming; but, generally, we know that ketamine works via the glutamate system to produce its effects [9]. Glutamate is an excitatory neurotransmitter, meaning it increases the firing rate of neurons after binding to receptors on the outside of another neuron. Glutamate interacts specifically with AMPA and NMDA receptors, as these two receptors have channels that allow positive charges to enter the cell and cause the neuron to fire when necessary. When glutamate binds to an AMPA receptor, it passes through a channel and then binds to an NMDA receptor. In this way, AMPA and NMDA receptors are linked: when AMPA receptors are activated, NMDA receptors become activated as well. However, this constant glutamate signaling mechanism is disrupted when ketamine is ingested; after ingestion, the drug binds to NMDA and blocks the receptor’s ability to be activated by glutamate. The remaining glutamate that can no longer bind to the NMDA receptor preferentially binds to the AMPA receptors, causing the neuron to fire or send an excitatory signal to other cells. This process, known as “direct binding,” is what sets ketamine treatment apart from traditional antidepressants like SSRIs. SSRIs merely increase the chance that a neurotransmitter will bind to a receptor. Ketamine administration, on the other hand, facilitates the direct binding of glutamate to receptors. And, because direct binding occurs more immediately than the indirect binding caused by SSRIs, the antidepressant effects of ketamine set in much quicker [9].
In addition to the speedy effects of direct binding, ketamine may also act more quickly than other drugs by facilitating neural plasticity, a construct typically associated with the way the brain changes to accommodate learning and memory. MDD has been associated with a breakdown in neuroplasticity, and recent findings have consequently linked the promotion of neuroplasticity with antidepressant effects [11]. In other words, since the disruption of neuroplasticity is thought to be the basic pathological mechanism underlying the disorder, the restoration of plasticity should ameliorate depression [13]. When ketamine binds to NMDA receptors, and AMPA receptors are activated in parallel, this AMPA activation increases the production of brain-derived neurotrophic factor (BDNF) [10]. BDNF is a protein that promotes the formation and strengthening of neuronal connections [12]. As these connections get stronger, neurons can send signals and relay information more quickly and effectively. These stronger neuronal connections react to ketamine much more quickly, leading to a more powerful antidepressant effect [12]. Further, ketamine may support neural plasticity by changing the structure of neurons themselves [4]. The neuron’s dendrites, which resemble the branches of a tree, have small protrusions called spines, which receive signals from other neurons. Spines increase the number of connections that the dendrite can make to other neurons; this measure is considered a direct indication of increased brain plasticity. Thus, ketamine differs from traditional antidepressants by restoring neuroplasticity lost through MDD and promoting the direct binding of glutamate for quick and effective enhancement of mood regulation. But what do these fascinating neural mechanisms of ketamine actually look like in practice? What behavioral or emotional changes can we observe in depression patients who try ketamine in medical trials?
What Makes “Special K” so Special?: The Therapeutic Properties of Ketamine in Action
First, contrary to what you might imagine recreational ketamine use to look like, employing ketamine as an antidepressant doesn’t mean that patients will be snorting lines in order to receive their treatment. In fact, initial studies administered ketamine to patients using an IV [5]. However, this method presented an accessibility issue: patients would be required to take hospital trips in order to receive treatment. Consequently, intranasal sprays have become the leading form of treatment administration. As of 2019, the FDA has approved an intranasal ketamine spray specifically for patients with treatment-resistant depression, as it was found to significantly reduce MDD symptoms such as fatigue and feelings of hopelessness [14]. However, this means that intranasal ketamine is currently only legal for depression patients after traditional treatments fail to provide any meaningful improvement [15]. Ketamine use has not yet been approved for all MDD patients; but, this may be subject to change in the coming years. With more and more findings pointing toward intranasal ketamine’s efficacy in reducing depressive symptoms, we may see a broadening of legal treatment criteria. This seems especially possible considering ketamine’s success as an antidepressant when compared with other treatments on the market.
As discussed earlier, ketamine works differently than other antidepressants, but it also may work better. Ketamine appears to represent a drastically safer and more effective option than our two currently well-established depression treatments: SSRIs and electroconvulsive therapy (ECT). ECT, which is most frequently administered in cases of treatment-resistant depression, uses electric currents to stimulate the brain. However, this treatment is controversial because it sometimes results in memory loss and other harmful symptoms [16]. Notably, ketamine treatment reduces symptoms of depression significantly more than both ECT and SSRIs, without these treatments’ dangerous side effects [14]. However, its unique success as an antidepressant is also rooted in its timeline of effectiveness.
One of the biggest drawbacks of SSRIs is that they take a long time to start showing behavioral effects, and these effects wear off very quickly. This makes the treatment process difficult as individuals have to wait upwards of two months to figure out if their medication works — not to mention that forgetting a single dose can lead to a relapse of symptoms [19]. In contrast, ketamine takes effect roughly two hours after administration, which is very exciting given that most current treatments do not show such a rapid onset of beneficial effects [18, 17]. Because ketamine acts so rapidly, we believe that it directly interacts with the biochemical pathway underlying depression. Ketamine is paradoxically known to have a relatively short half-life, meaning that it doesn’t take long for its active components to leave the body, despite it having incredibly long-lasting effects [17]. This phenomenon suggests that when ketamine binds to receptors, it alters some aspect of the brain, which causes effects to continue long after the drug has left the body [17]. Most traditional antidepressants require daily intake because they cause temporary alterations to neurotransmitter concentrations, rather than causing permanent alterations to the brain itself. But, this long-lasting property of ketamine would mean less frequent doses are needed. Therefore, in comparison to current treatment options, ketamine appears to be remarkably more effective because of its fast action and longevity.
Is Special K Coming to a Clinic Near You?: Addressing Ketamine Treatment Uncertainties
So, it’s clear that ketamine shows great promise as a treatment for MDD, but how long will it take for this new antidepressant to gain widespread acceptance? Scientists are quite confident that ketamine will be a successful treatment option; but, only if it manages to overcome all the hurdles that stand in its way. One of the biggest obstacles to ketamine treatment implementation is the social stigma surrounding the drug. How can a popular club drug become a useful treatment for something as serious as MDD? There is already a stigma surrounding antidepressants as a whole, and adding ketamine into the mix is a turn-off for many patients [20]. Many believe that the widespread legalization of the drug as a depression treatment could help reduce the stigma surrounding it [20]. However, even with legalization, many patients may still be hesitant to try ketamine treatment due to its uncertain long-term effects. While short-term use of ketamine as an antidepressant has proven to be safe, there is currently not much research on the effects of long-term use, including the potential for addiction. Ketamine can be an addictive drug, which may pose problems if ketamine therapy becomes a long-term treatment option [21]. Consequently, many MDD patients who are considering the use of ketamine are interested in implementing additional monitoring if they choose this treatment route. Knowing that someone is following their progress reduces the anxiety that many MDD patients feel about the safety of their at-home ketamine treatment [20, 21]. Therefore, while some apprehension surrounding ketamine treatment exists, there are also creative ways of addressing patient concerns.
Similarly, despite these hurdles, many of the thousands of people who struggle to find respite from their depression symptoms remain hopeful for ketamine’s legalization [21, 20]. In 2020, a chemical cousin of ketamine, esketamine, was approved by the FDA for MDD patients experiencing acute suicidal ideations or behaviors; this decision was essential as it broadened the drug’s previous legal usage criteria from only individuals with treatment-resistant depression [22]. Still, these treatments are currently only approved for use in clinical settings, so they are not yet ready to be implemented as a common practice [22]. More research on the long-term effects and development of protocols to maintain patient safety will be needed before we see this drug become the new and improved, common antidepressant. Hopefully, people who suffer from depression will soon be able to experience the miraculous benefits of this “special” and unexpected treatment.
REFERENCES
Hashimoto, K. (2019). Rapid-acting antidepressant ketamine, its metabolites and other candidates: A historical overview and future perspective. Psychiatry and Clinical Neurosciences, 73(10), 613-627. doi:10.1111/pcn.12902
Shin, C., & Kim, Y-K. (2020). Ketamine in major depressive disorder: Mechanisms and future perspectives. Psychiatry Investigation, 17(3), 181-192. doi:10.30773/pi.2019.0236
National Institute of Mental Health. (2019). Major depression. National Institute of Mental Health. Retrieved from https://www.nimh.nih.gov/health/statistics/major-depression.shtml
Li, L., & Vlisides, P. E. (2016). Ketamine: 50 years of modulating the mind. Frontiers In Human Neuroscience, 10(612), 1-15. doi:10.3389/fnhum.2016.00612
Berman, R. M., Cappiello, A., Anand, A., Oren, D. A., Heninger, G. R., Charney, D. S., & Krystal, J. H. (2020). Antidepressant effects of ketamine in depressed patients. Biological Psychiatry, 47(4), 351–354. doi:10.1016/s0006-3223(99)00230-9
Skolnick, P., Layer, R. T., Popik, P., Nowak, G., Paul, I., & Trullas, R. (1996). Adaptation of N-methyl-D-aspartate (NMDA) receptors following antidepressant treatment: Implications for the pharmacotherapy of depression. Pharmacopsychiatry, 29(1), 23–26. doi:10.1055/s-2007-979537
Reinstatler, L., & Youssef, N. A. (2015). Ketamine as a potential treatment for suicidal ideation: A systematic review of the literature. Drugs in R&D, 15(1), 37–43. doi:10.1007/s40268-015-0081-0
Murrough J. W. (2012). Ketamine as a novel antidepressant: From synapse to behavior. Clinical Pharmacology and Therapeutics, 91(2), 303–309. doi:10.1038/clpt.2011.244
Maeng, S., & Zarate, C. A., Jr (2007). The role of glutamate in mood disorders: Results from the ketamine in major depression study and the presumed cellular mechanism underlying its antidepressant effects. Current Psychiatry Reports, 9(6), 467–474. doi:10.1007/s11920-007-0063-1
Sleigh, J., Harvey, M., Voss, L., & Denny, B. (2014). Ketamine—more mechanisms of action than just NMDA blockade. Trends in Anaesthesia and Critical Care, 4(2), 76-81. doi:10.1016/j.tacc.2014.03.002
Aleksandrova, L. R., & Phillips, A. G. (2021). Neuroplasticity as a convergent mechanism of ketamine and classical psychedelics. Trends in Pharmacological Sciences, 42(11). doi:10.1016/j.tips.2021.08.003
Autry, A., Adachi, M., Nosyreva, E., Na, E. S., Maarten, F. L., Cheng, P., Kavalali, E. T., & Monteggia, L. M. (2011). NMDA receptor blockade at rest triggers rapid behavioural antidepressant responses. Nature, 475, 91–95. doi:10.1038/nature10130
Liu, W., Ge, T., Leng, Y., Pan, Z., Fan, J., Yang, W., & Cui, R. (2017). The role of neural plasticity in depression: From hippocampus to prefrontal cortex. Neural Plasticity, 2017(6871089). doi:10.1155/2017/6871089
Ghasemi, M., Kazemi, M. H., Yoosefi, A., Ghasemi, A., Paragomi, P., Amini, H., & Afzali, M. H. (2014). Rapid antidepressant effects of repeated doses of ketamine compared with electroconvulsive therapy in hospitalized patients with major depressive disorder. Psychiatry Research, 215(2), 355-361. doi:10.1016/j.psychres.2013.12.008
Daly, E. J., Singh, J. B., Fedgchin, M., Cooper, K., Lim, P., Shelton, R. C., Thase, M. E., Winokur, A., Van Nueten, L., Manji, H., & Drevets, W. C. (2018). Efficacy and safety of intranasal esketamine adjunctive to oral antidepressant therapy in treatment-resistant depression: A randomized clinical trial. JAMA Psychiatry, 75(2), 139-148. doi:10.1001/jamapsychiatry.2017.3739
Vasavada, M. M., Leaver, A. M., Njau, S., Joshi, S. H., Ercoli, L., Hellemann, G., Narr, K. L., & Espinoza, R. (2017). Short- and long-term cognitive outcomes in patients with major depression treated with electroconvulsive therapy. The Journal of ECT, 33(4), 278–285. doi:10.1097/YCT.0000000000000426
Brachman, R. A., McGowan, J. C., Perusini, J. N., Lim, S. C., Pham, T. H., Faye, C., Gardier, A. M., Mendez-David, I., David, D. J., Hen, R., & Denny, C. A. (2016). Ketamine as a prophylactic against stress-induced depressive-like behavior. Biological Psychiatry, 79(9), 776-786. doi:10.1016/j.biopsych.2015.04.022
Hasselmann H. W. (2014). Ketamine as antidepressant? Current state and future perspectives. Current Neuropharmacology, 12(1), 57–70. doi:10.2174/1570159X113119990043
Chouinard, G., & Chouinard, V. A. (2015). New classification of selective serotonin reuptake inhibitor withdrawal. Psychotherapy and Psychosomatics, 84(2), 63-71. doi:10.1159/000371865
Jilka, S., Odoi, C. M., Wilson, E., Meran, S., Simblett, S., & Wykes, T. (2021). Ketamine treatment for depression: Qualitative study exploring patient views. BJPsych open, 7(1), e32. doi:10.1192/bjo.2020.165
Jilka, S., Murray, C., Wieczorek, A., Griffiths, H., Wykes, T., & McShane, R. (2019). Exploring patients’ and carers’ views about the clinical use of ketamine to inform policy and practical decisions: Mixed-methods study. BJPsych Open, 5(5), e62. doi:10.1192/bjo.2019.52
Sapkota, A., Khurshid, H., Qureshi, I. A., Jahan, N., Went, T. R., Sultan, W., & Alfonso, M. (2021). Efficacy and safety of intranasal esketamine in treatment-resistant depression in adults: A systematic review. Cureus, 13(8). doi:10.7759/cureus.17352